Obamacare cash fuels healthcare merger mania
A gusher of Obamacare money is fueling a merger frenzy in U.S. healthcare.
The latest jolt came Thursday when Woodland Hills insurer Health Net Inc. agreed to be bought by Medicaid insurer Centene Corp. for $6.8 billion.
And more billion-dollar deals are in the works as health insurers, hospitals and drug companies bulk up in size so they can seize on government spending in Obamacare exchanges, state Medicaid programs and Medicare Advantage for the baby boomers.
Riding high on Wall Street and flush with cash, big health insurers in particular have been on the prowl for deals. Atop the shopping list are companies that boost their government business.
“The Affordable Care Act is really driving this merger mania,” said Gerald Kominski, director of the UCLA Center for Health Policy Research. “There are billions of dollars pouring into the system, and it’s money to buy insurance.”
President Obama’s signature health law has unleashed the biggest expansion of insurance coverage in half a century, lifting stock prices and revenues across the healthcare industry.
Medical companies cheered the Supreme Court ruling last week that kept the spigot turned on by upholding the premium subsidies that millions of Americans rely on to make coverage affordable.
The federal government is expected to spend $1.2 trillion over the next decade on subsidies and other aspects of the health law.
Nearly 17 million Americans have gained health insurance since September 2013, and billions of dollars in uncompensated care has been wiped out for hospitals that are seeing more paying patients.
Despite all those gains, some regulators and consumer advocates expressed alarm about this increasing consolidation. They worry that this will create powerful new healthcare giants that will limit the negotiating power of government health programs and employers to hold down prices.
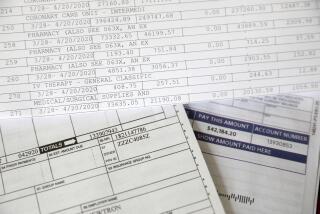
They fear that the nation’s $3-trillion healthcare tab will keep growing uncontrollably, putting a squeeze on government budgets and the pocketbooks of everyday Americans.
“We cannot afford what we are paying now,” said Glenn Melnick, a healthcare economist and professor at USC. “Healthcare could eat up the federal budget.”
Workers’ share of employer health premiums soared 93% in the last decade at a time of relatively little wage growth, according to the Commonwealth Fund, a New York think tank.
The supersized insurers say not to worry. They insist that they will be able to use their big numbers to win better terms and lower prices from hospitals, doctors and drugmakers.
But some experts are skeptical that this industry arms race will address the underlying problems with wasteful medical spending, which accounts for up to 30% of overall costs by some estimates.
“It’s not entirely clear the savings get passed on to consumers,” UCLA’s Kominski said.
There are also concerns about whether government officials are doing enough to hold health insurers accountable for providing adequate access to care. A recent audit criticized California officials for a lack of oversight on private insurers running Medicaid HMOs.
The latest deal involves Health Net, California’s fourth-largest health insurer. It is prized for its big presence in California’s Medicaid program, known as Medi-Cal, where its serves nearly 1.4 million residents.
Medi-Cal is the nation’s largest Medicaid program with 12.5 million people enrolled.
Almost 1 in 3 Californians now get coverage through the state’s insurance program for the poor, and many of them have been moved to managed-care plans run by private insurers in a bid to save money.
After the merger, Centene said it expects to become one of the largest Medicaid health insurers in the country with about 6 million members.
“Centene is the largest Medicaid managed-care company but has only minor market share in California, where Health Net has been rapidly growing in Medicaid,” said Peter Costa, a senior healthcare analyst at Wells Fargo. “Centene and Health Net don’t desire to be left out of the consolidation wave.”
Health Net shares rallied on the news, jumping $6.51, or 10%, to $71.57 on Thursday. Centene’s offer of $78.57 a share was a 21% premium over Health Net’s closing price Wednesday. The cash-and-stock deal includes the assumption of $500 million in debt.
Centene shares fell after the deal was announced, closing down $6.46, or 8%, at $74.44.
Overall, investors in the healthcare sector have been well rewarded. Shares of healthcare companies have surged 24% in the last year — three times the increase in the broader Standard & Poor’s 500 stock index.
Some analysts said it was still possible that a bidding war could erupt for Health Net in the coming weeks.
UnitedHealth Group Inc., Anthem Inc. and other major insurers have all been looking for merger partners in recent weeks.
Cigna Corp. has rejected a $54-billion offer from Anthem, the nation’s second-largest health insurer, but those talks are continuing. Analysts also expect Aetna Inc. to scoop up rival Humana Inc., which has a big Medicare Advantage business.
Analysts also expect Aetna Inc. to scoop up rival Humana Inc., which has a big Medicare Advantage business.
“We expect UnitedHealth could come in with a competing bid for either Health Net or Centene or both,” said Ana Gupte, a healthcare analyst at Leerink Partners.
Both Health Net and Centene declined to comment on that prospect.
Michael Neidorff, Centene’s chairman and chief executive, would hold those jobs after the merger. Jay Gellert, Health Net’s CEO, said he would assist in the transition.
The company would be based in St. Louis. That would make Health Net the latest of several companies whose corporate headquarters have left Southern California.
Health Net officials cautioned that it was too early to know the outcome for its 2,500 employees at the Woodland Hills office. Overall, the company has 8,300 workers.
The dealmaking could spread to Long Beach insurer Molina Healthcare Inc., another Medicaid insurer that is active in many states.
J. Mario Molina, the company’s CEO, said he couldn’t comment directly on the rumors.
“The Aetnas, Humanas and Anthems of the world are going to be the bigger players. All that has to sort itself out,” he said. “It’s a wild time.”
Twitter: @chadterhune